Our Health Library information does not replace the advice of a doctor. Please be advised that this information is made available to assist our patients to learn more about their health. Our providers may not see and/or treat all topics found herein.
Burns and Electric Shock
Overview
Most burns are minor injuries that occur at home or work. It's common to get a minor burn from hot water, a curling iron, or touching a hot stove. Home treatment is usually all that's needed for healing and to prevent other problems, such as infection.
There are many types of burns.
- Heat burns (thermal burns) are caused by fire, steam, hot objects, or hot liquids. Scald burns from hot liquids are the most common burns to children and older adults.
- Cold temperature burns are caused by skin exposure to wet, windy, or cold conditions. They can also be caused by touching cold items such as dry ice without protection.
- Electrical burns are caused by contact with electrical sources or by lightning.
- Chemical burns are caused by contact with household or industrial chemicals in a liquid, solid, or gas form, such as acids. Natural foods such as chili peppers, which contain a substance that irritates the skin, can cause a burning sensation.
- Radiation burns are caused by the sun, tanning booths, sunlamps, X-rays, or radiation therapy for cancer treatment.
- Friction burns are caused by contact with any hard surface such as roads ("road rash"), carpets, or gym floor surfaces. They are usually both a scrape (abrasion) and a heat burn.
Breathing in hot air or gases can injure your lungs (inhalation injuries).
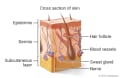
Burns injure the skin layers. They can also injure other parts of the body, such as muscles, blood vessels, nerves, lungs, and eyes. Burns are defined as first-, second-, third-, or fourth-degree, depending on how many layers of skin and tissue are burned. The deeper the burn and the larger the burned area, the more serious the burn is.
- First-degree burns are burns of the first layer of skin.
- There are two types of second-degree burns:
- Superficial partial-thickness burns injure the first and second layers of skin.
- Deep partial-thickness burns injure deeper skin layers.
- Third-degree burns (full-thickness burns) injure all the skin layers and tissue under the skin. These burns always require medical treatment.
- Fourth-degree burns extend through the skin to injure muscle, ligaments, tendons, nerves, blood vessels, and bones. These burns always require medical treatment.
How serious a burn is depends on several things, such as:
- The depth, size, and cause of the burn; the affected body area; and the age and health of the burn victim.
- Any other injuries that occurred, and the need for follow-up care.
Burns in children
Babies and young children may have a more severe reaction from a serious burn than an adult. A burn in an adult may cause a minor loss of fluids from the body. But in a baby or young child, the same size and depth of a burn may cause a severe fluid loss.
How safe a child's environment needs to be depends on the child's age and how much the child needs to be supervised. At each stage of a child's life, look for burn hazards. Then use appropriate safety measures to keep things out of a child's reach. Since most burns happen in the home, simple safety measures decrease the chance of anyone getting burned.
When a child or vulnerable adult is burned, it's important to find out how the burn happened. If the reported cause of the burn doesn't match how the burn looks, it may be a sign of abuse. In that case, resources for help, such as social services, are offered. Self-inflicted burns will need treatment as well as an evaluation of the person's emotional health.
Infection
Infection is a concern with all burns. Watch for signs of infection during the healing process. Home treatment for a minor burn will reduce the risk of infection. Deep burns with open blisters are more likely to get infected and need medical treatment.
Check Your Symptoms
The medical assessment of symptoms is based on the body parts you have.
- If you are transgender or nonbinary, choose the sex that matches the body parts (such as ovaries, testes, prostate, breasts, penis, or vagina) you now have in the area where you are having symptoms.
- If your symptoms aren’t related to those organs, you can choose the gender you identify with.
- If you have some organs of both sexes, you may need to go through this triage tool twice (once as "male" and once as "female"). This will make sure that the tool asks the right questions for you.
Many things can affect how your body responds to a symptom and what kind of care you may need. These include:
- Your age. Babies and older adults tend to get sicker quicker.
- Your overall health. If you have a condition such as diabetes, HIV, cancer, or heart disease, you may need to pay closer attention to certain symptoms and seek care sooner.
- Medicines you take. Certain medicines, such as blood thinners (anticoagulants), medicines that suppress the immune system like steroids or chemotherapy, herbal remedies, or supplements can cause symptoms or make them worse.
- Recent health events, such as surgery or injury. These kinds of events can cause symptoms afterwards or make them more serious.
- Your health habits and lifestyle, such as eating and exercise habits, smoking, alcohol or drug use, sexual history, and travel.
Try Home Treatment
You have answered all the questions. Based on your answers, you may be able to take care of this problem at home.
- Try home treatment to relieve the symptoms.
- Call your doctor if symptoms get worse or you have any concerns (for example, if symptoms are not getting better as you would expect). You may need care sooner.
It can be hard to tell how deep a burn is.
- A fourth-degree burn goes through the skin and fatty tissue to injure muscle, nerves, blood vessels, and bones.
- A third-degree burn goes through all the skin layers to the fatty tissue beneath. The skin is dry and swollen and may be pale white or charred black. This kind of burn destroys the nerves, so it may not hurt except on the edges.
- A second-degree burn involves several layers of skin. The skin may be swollen, puffy, moist, or blistered.
- A first-degree burn affects only the outer layer of skin. The skin is dry and hurts when you touch it. A mild sunburn is a first-degree burn.
Some common burn patterns and common areas for burns that result from abuse include:
- Circular burns that are the size and shape of the end of a cigarette or cigar.
- Burns on the bottom of the feet.
- Burns that look like gloves (on the hands), socks (on the feet), or a large circle on the buttocks. These come from putting someone's hands, feet, or buttocks in a sink or tub of scalding-hot water.
With burns caused by abuse, the explanation for the burn may not match the size, shape, or location of the burn. But it still can be hard to tell whether a burn was caused on purpose. A burn caused by throwing hot liquid on someone may look just like a burn caused by an accidental spill.
Symptoms of difficulty breathing can range from mild to severe. For example:
- You may feel a little out of breath but still be able to talk (mild difficulty breathing), or you may be so out of breath that you cannot talk at all (severe difficulty breathing).
- It may be getting hard to breathe with activity (mild difficulty breathing), or you may have to work very hard to breathe even when you’re at rest (severe difficulty breathing).
Severe trouble breathing means:
- The child cannot eat or talk because he or she is breathing so hard.
- The child's nostrils are flaring and the belly is moving in and out with every breath.
- The child seems to be tiring out.
- The child seems very sleepy or confused.
Moderate trouble breathing means:
- The child is breathing a lot faster than usual.
- The child has to take breaks from eating or talking to breathe.
- The nostrils flare or the belly moves in and out at times when the child breathes.
Mild trouble breathing means:
- The child is breathing a little faster than usual.
- The child seems a little out of breath but can still eat or talk.
Severe trouble breathing means:
- You cannot talk at all.
- You have to work very hard to breathe.
- You feel like you can't get enough air.
- You do not feel alert or cannot think clearly.
Moderate trouble breathing means:
- It's hard to talk in full sentences.
- It's hard to breathe with activity.
Mild trouble breathing means:
- You feel a little out of breath but can still talk.
- It's becoming hard to breathe with activity.
Heartbeat changes can include:
- A faster or slower heartbeat than is normal for you. This would include a pulse rate of more than 120 beats per minute (when you are not exercising) or less than 50 beats per minute (unless that is normal for you).
- A heart rate that does not have a steady pattern.
- Skipped beats.
- Extra beats.
Pain in adults and older children
- Severe pain (8 to 10): The pain is so bad that you can't stand it for more than a few hours, can't sleep, and can't do anything else except focus on the pain.
- Moderate pain (5 to 7): The pain is bad enough to disrupt your normal activities and your sleep, but you can tolerate it for hours or days. Moderate can also mean pain that comes and goes even if it's severe when it's there.
- Mild pain (1 to 4): You notice the pain, but it is not bad enough to disrupt your sleep or activities.
Pain in children under 3 years
It can be hard to tell how much pain a baby or toddler is in.
- Severe pain (8 to 10): The pain is so bad that the baby cannot sleep, cannot get comfortable, and cries constantly no matter what you do. The baby may kick, make fists, or grimace.
- Moderate pain (5 to 7): The baby is very fussy, clings to you a lot, and may have trouble sleeping but responds when you try to comfort him or her.
- Mild pain (1 to 4): The baby is a little fussy and clings to you a little but responds when you try to comfort him or her.
Here are some ways to estimate how much of the body is burned in an adult or older child.
- The palm of the person's hand equals 1% of the body's surface area. Using the person's palm is a good way to estimate the size of a small burn.
- The total surface of the head plus the neck is 9% of the body's surface area.
- The total surface of one arm and hand is 9%.
- The chest is 9%.
- The belly is 9%.
- The upper back is 9%.
- The lower back is 9%.
- The total surface of one leg and foot is 18%.
- The groin area is 1%.
Here are some ways to estimate how much of the body is burned in a baby or young child.
- The palm of the child's hand equals 1% of the body's surface area. Using the child's palm is a good way to estimate the size of a small burn.
- The total surface of the head plus the neck is 21% of the body's surface area.
- The total surface of one arm and hand is 10%.
- The total surface of the chest plus the belly is 13%.
- The back is 13%.
- The buttocks are 5%.
- The total surface of one leg and foot is 13.5%.
- The groin area is 1%.
Symptoms of infection may include:
- Increased pain, swelling, warmth, or redness in or around the area.
- Red streaks leading from the area.
- Pus draining from the area.
- A fever.
Certain health conditions and medicines weaken the immune system's ability to fight off infection and illness. Some examples in adults are:
- Diseases such as diabetes, cancer, heart disease, and HIV/AIDS.
- Long-term alcohol and drug problems.
- Steroid medicines, which may be used to treat a variety of conditions.
- Chemotherapy and radiation therapy for cancer.
- Other medicines used to treat autoimmune disease.
- Medicines taken after organ transplant.
- Not having a spleen.
Shock is a life-threatening condition that may quickly occur after a sudden illness or injury.
Adults and older children often have several symptoms of shock. These include:
- Passing out (losing consciousness).
- Feeling very dizzy or lightheaded, like you may pass out.
- Feeling very weak or having trouble standing.
- Not feeling alert or able to think clearly. You may be confused, restless, fearful, or unable to respond to questions.
Shock is a life-threatening condition that may occur quickly after a sudden illness or injury.
Babies and young children often have several symptoms of shock. These include:
- Passing out (losing consciousness).
- Being very sleepy or hard to wake up.
- Not responding when being touched or talked to.
- Breathing much faster than usual.
- Acting confused. The child may not know where he or she is.
To clean a wound well:
- Wash your hands first.
- Remove large pieces of dirt or debris from the wound with cleaned tweezers. Do not push the tweezers deeply into the wound.
- Hold the wound under cool running water. If you have a sprayer in your sink, you can use it to help remove dirt and other debris from the wound.
- Scrub gently with water, a mild soap, and a washcloth.
- If some dirt or other debris is still in the wound, clean it again.
- If the wound starts to bleed, put direct, steady pressure on it.
If a chemical has caused a wound or burn, follow the instructions on the chemical's container or call Poison Control (1-800-222-1222) to find out what to do. Most chemicals should be rinsed off with lots of water, but with some chemicals, water may make the burn worse.
Usually found in dirt and soil, tetanus bacteria typically enter the body through a wound. Wounds may include a bite, a cut, a puncture, a burn, a scrape, insect bites, or any injury that may cause broken skin.
You may need a tetanus shot depending on how dirty the wound is and how long it has been since your last shot.
- For a dirty wound that has things like dirt, saliva, or feces in it, you may need a shot if:
- You haven't had a tetanus shot in the past 5 years.
- You don't know when your last shot was.
- For a clean wound, you may need a shot if:
- You have not had a tetanus shot in the past 10 years.
- You don't know when your last shot was.
Seek Care Today
Based on your answers, you may need care soon. The problem probably will not get better without medical care.
- Call your doctor today to discuss the symptoms and arrange for care.
- If you cannot reach your doctor or you don't have one, seek care today.
- If it is evening, watch the symptoms and seek care in the morning.
- If the symptoms get worse, seek care sooner.
Seek Care Now
Based on your answers, you may need care right away. The problem is likely to get worse without medical care.
- Call your doctor now to discuss the symptoms and arrange for care.
- If you cannot reach your doctor or you don't have one, seek care in the next hour.
- You do not need to call an ambulance unless:
- You cannot travel safely either by driving yourself or by having someone else drive you.
- You are in an area where heavy traffic or other problems may slow you down.
Call 911 Now
Based on your answers, you need emergency care.
Call 911 or other emergency services now.
Sometimes people don't want to call 911. They may think that their symptoms aren't serious or that they can just get someone else to drive them. Or they might be concerned about the cost. But based on your answers, the safest and quickest way for you to get the care you need is to call 911 for medical transport to the hospital.
Make an Appointment
Based on your answers, the problem may not improve without medical care.
- Make an appointment to see your doctor in the next 1 to 2 weeks.
- If appropriate, try home treatment while you are waiting for the appointment.
- If symptoms get worse or you have any concerns, call your doctor. You may need care sooner.
Self-Care
First aid for burns
If you think that you might have a severe burn, use these first-aid measures while you arrange to be seen by your doctor.
- First, stop the burning to prevent a more severe burn.
- Heat burns (thermal burns).
Smother any flames by covering them with a blanket or water. If your clothing catches fire, don't run. Stop, drop, and roll on the ground to smother the flames.
- Cold temperature burns.
Try to warm the areas. Small areas of your body (ears, face, nose, fingers, toes) that are really cold or frozen can be warmed by blowing warm air on them, tucking them inside your clothing, or putting them in warm water. Don't rub or massage frozen skin.
- Liquid scald burns (thermal burns).
Run cool tap water over the burn for 10 to 20 minutes. Don't use ice.
- Electrical burns.
After the person has been separated from the electrical source, check for breathing and a heartbeat. If the person isn't breathing or doesn't have a heartbeat, call 911.
- Chemical burns.
When a chemical burn occurs, find out what chemical caused the burn. Call your local Poison Control Center or the National Poison Control Hotline (1-800-222-1222) for more information about how to treat the burn. Natural foods such as chili peppers, which contain a substance that irritates the skin, can cause a burning sensation.
- Tar or hot plastic burns.
Run cold water over the hot tar or hot plastic right away. It will cool the tar or plastic.
- Next, look for other injuries. The burn may not be the only injury.
- Remove any jewelry or clothing at the site of the burn.
If clothing is stuck to the burn, don't remove it. Carefully cut around the stuck fabric to remove loose fabric. Remove all jewelry, because it may be hard to remove it later if swelling occurs.
- Prepare to be seen by a doctor.
If you are going to see your doctor soon:
- Cover the burn with a clean, dry cloth to reduce the risk of infection.
- Don't put any salve or medicine on the burned area, so your doctor can properly assess your burn.
- Don't put ice on the burned area. It doesn't help, and it can damage the skin tissue.
Caring for a minor burn
Here are things you can do at home for minor burns, such as first-degree burns or sunburns.
- Use cool cloths on burned areas.
- Take frequent cool showers or baths.
- Apply moisturizing lotions or creams.
These skin lotions can be used to relieve itching. But don't use them if the burns have fluid weeping from them or have fresh scabs.
There isn't much you can do to stop skin from peeling after a sunburn—it's part of the healing process. Lotion may help relieve the itching.
- Try other remedies.
There isn't clear proof that other common remedies are safe and effective, but they may help. For example, you can use an aloe vera lotion or gel, apply calamine lotion for itching, or try an oatmeal bath product, such as Aveeno.
- Try medicine.
- Using 0.5% hydrocortisone cream on the burned area may help. You will need to check with your doctor first if you need to use the cream for a child younger than age 2 or for use in the genital area.
- An antihistamine may help stop itching. Be safe with medicines. Read and follow all instructions on the label.
- Protect burns while they heal.
Newly healed burns can be sensitive to temperature. Healing burns need to be protected from the cold, because the burned area is more likely to develop frostbite. And a newly burned area can sunburn easily. Protect the new skin from sun exposure for the first year after a burn. You can do this by covering the new skin with clothing, staying in the shade, or using sunscreen.
- Don't smoke.
Smoking slows healing because it decreases blood supply and delays tissue repair.
Caring for a chemical burn
Not all chemical burns are treated with water. Follow the instructions below to care for those other types of burns.
- Carbolic acid or phenol burns. Use isopropyl (rubbing) alcohol first to flush the chemical off the skin. Then flush with water. If alcohol isn't available, flush with a large amount of water. Do not flush the eye with alcohol.
- Sulfuric acid burns. Flush with a mild, soapy solution if the burns aren't severe. Sulfuric acid feels hot when water is added to the acid. But it's better to flush the area and not leave the acid on the skin.
- Dry powder burns. Brush the powder away first. That's because adding water can make a liquid that burns. After the powder is brushed away, flush with water for 20 minutes. Lime is an example of a dry powder burn.
- Metal compound burns. Cover these burns with mineral oil.
A chemical burn can be caused by alkaline or acid products, metals, and hydrocarbons, such as gas.
Most chemical burns of the skin are treated first by rinsing (flushing) the chemical off your body with a large amount of water. It's important to treat the burn correctly to avoid further problems.
This is general information for treating a chemical burn. Call a Poison Control Center for more specific information.
If someone has swallowed a chemical that may be a poison or that may cause burning in the throat and esophagus, call your local Poison Control Center or the National Poison Control Hotline (1-800-222-1222) right away for information on treatment. When you call the Poison Control Center, have the chemical container with you, so you can read the content label to the Poison Control staff member. The Poison Control Center can help determine what steps to take next.
- Flush the area with water.
- Flush for at least 20 minutes. Don't use a hard spray of water. It can damage the burned area.
- Have the person with the burn remove the chemical substance if he or she is able.
- Put on gloves to protect yourself from the chemical, if you need to remove it.
- Remove anything that the chemical may be on.
As you flush the area, take off any clothing or jewelry that has the chemical on it.
- Continue to flush, if needed.
If the area still has a burning sensation after 20 minutes, flush the area again with flowing water for 10 to 15 minutes.
If you need to see a doctor for the burn, take the chemical container with you.
Caring for an electrical burn
Rinse the burns with water, and apply a bandage. There may be burns where the electrical current entered the body and where it left the body. If you have a visible electrical burn to the skin, an evaluation by your doctor is usually needed.
Caring for a tar or plastic burn
- Run cold water over the hot tar or hot plastic right away.
This helps stop the burning.
- Do not attempt to peel the tar or plastic off after it has cooled.
This may remove skin that is stuck to the tar or plastic.
- Loosen the tar or plastic with mineral oil or ointments such as Vaseline or Polysporin.
This can help remove the tar or plastic. Tar will likely peel off after a few days as the skin cells below the tar flake off normally.
- Wash and treat the burned skin after the tar or plastic is removed.
If you have any trouble removing tar or plastic from the skin, you need an evaluation by a doctor.
When to call for help during self-care
Call a doctor if any of the following occur during self-care at home:
- New or worse trouble breathing.
- New or worse pain.
- New or worse signs of infection, such as redness, warmth, swelling, pus, or a fever.
- Symptoms occur more often or are more severe.
Learn more
Preparing For Your Appointment
You can help your doctor diagnose and treat your condition by being prepared for your appointment.
Related Information
Credits
Current as of: November 16, 2023
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
Current as of: November 16, 2023
Author: Ignite Healthwise, LLC Staff
Clinical Review Board
All Healthwise education is reviewed by a team that includes physicians, nurses, advanced practitioners, registered dieticians, and other healthcare professionals.
This information does not replace the advice of a doctor. Ignite Healthwise, LLC disclaims any warranty or liability for your use of this information. Your use of this information means that you agree to the Terms of Use and Privacy Policy. Learn how we develop our content.
To learn more about Ignite Healthwise, LLC, visit webmdignite.com.
© 2024 Ignite Healthwise, LLC.